Navigating the Hormonal Rollercoaster: Acne Treatment During Menopause
Related Articles: Navigating the Hormonal Rollercoaster: Acne Treatment During Menopause
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Navigating the Hormonal Rollercoaster: Acne Treatment During Menopause. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Navigating the Hormonal Rollercoaster: Acne Treatment During Menopause

Menopause, a natural transition in a woman’s life, often brings with it a cascade of hormonal changes. While many women experience hot flashes, mood swings, and sleep disturbances, a less discussed yet significant symptom is the resurgence of acne. This seemingly paradoxical occurrence, often referred to as "menopausal acne," can be a source of frustration and discomfort. Understanding the underlying causes and effective treatment options is crucial for navigating this stage of life with confidence and clarity.
The Hormonal Connection: Unveiling the Root Cause
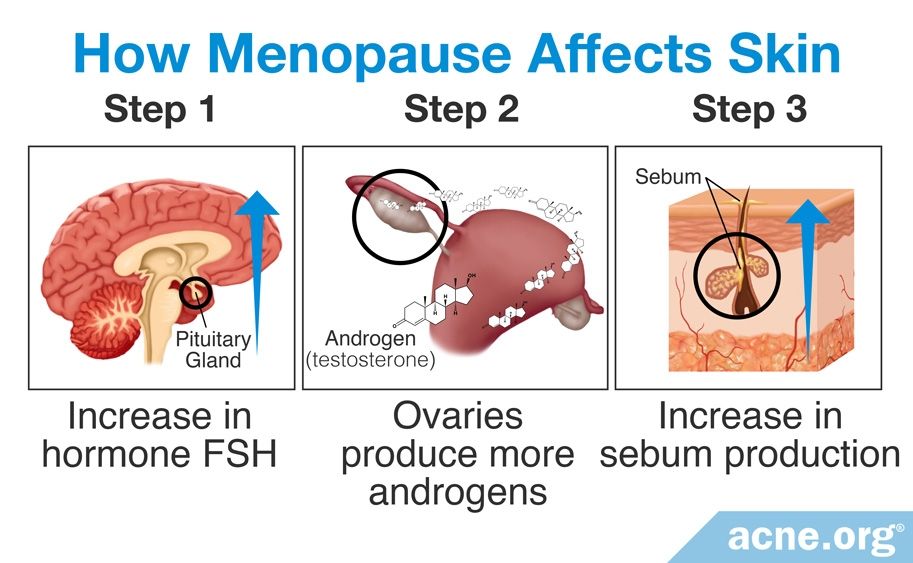
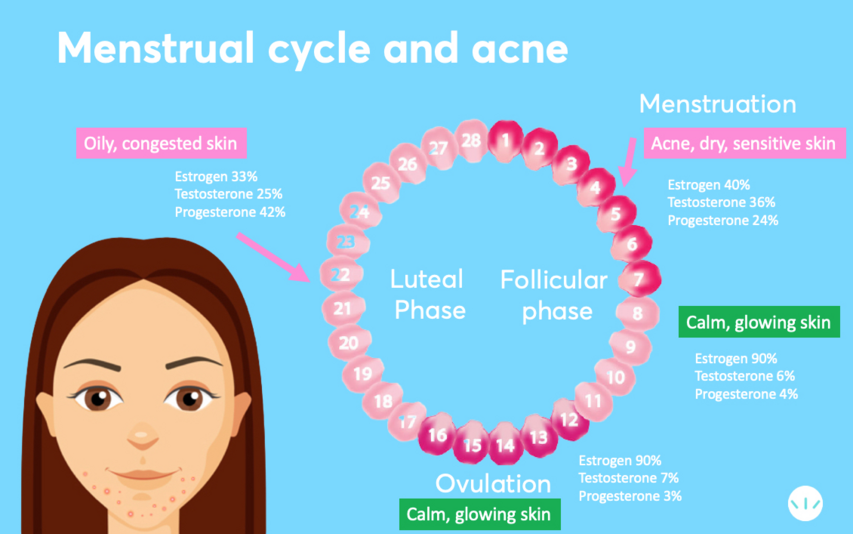
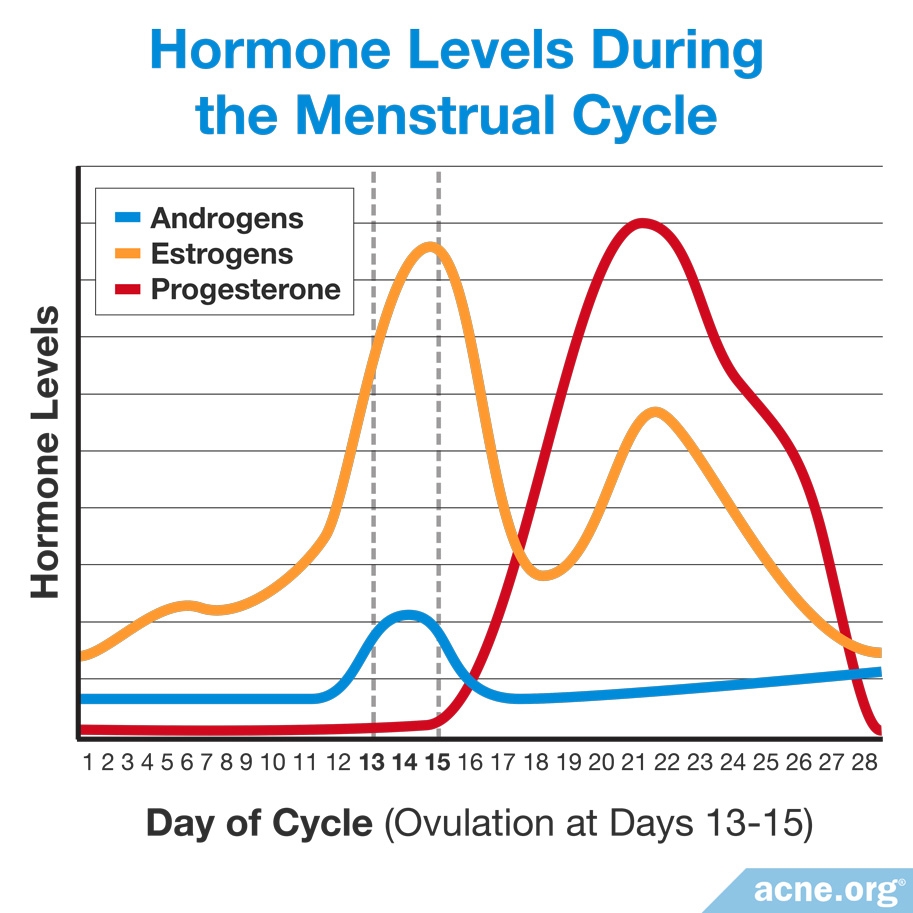
The primary culprit behind menopausal acne is the fluctuating levels of estrogen and progesterone. During menopause, the ovaries gradually cease production of these hormones, leading to an imbalance. This hormonal shift can trigger several changes in the skin:
- Increased sebum production: Estrogen normally helps regulate sebum (oil) production in the skin. With declining estrogen levels, the skin’s oil glands become more active, leading to excessive sebum secretion. This excess oil can clog pores, creating a breeding ground for bacteria and acne.
- Thickening of the skin: Progesterone also plays a role in skin health. During menopause, its decline can contribute to thicker skin, which can further impede the natural shedding of dead skin cells, exacerbating clogged pores.
- Inflammation: Hormonal fluctuations can trigger inflammation, making the skin more sensitive and prone to breakouts.
Navigating Treatment Options: A Comprehensive Approach
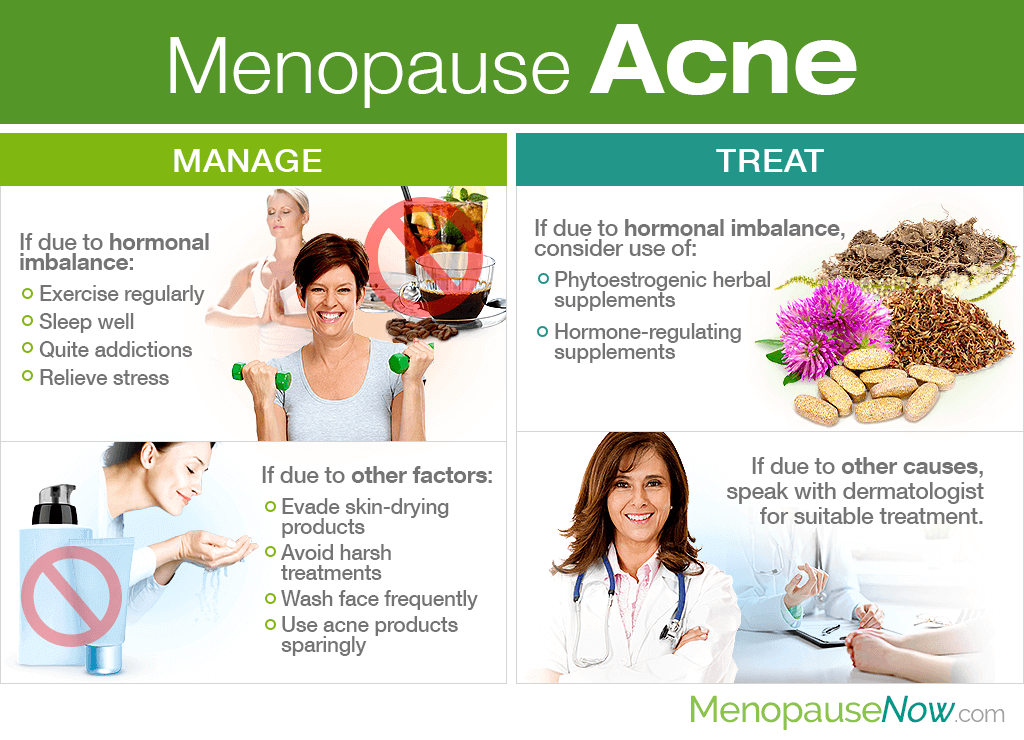
Addressing menopausal acne requires a multi-faceted approach that combines lifestyle modifications, over-the-counter (OTC) solutions, and, in some cases, prescription treatments.
1. Lifestyle Modifications: Building a Foundation for Clear Skin
- Cleanse gently: Opt for gentle, non-comedogenic (non-pore-clogging) cleansers to remove dirt, makeup, and excess oil without irritating the skin. Avoid harsh scrubs or soaps that can strip the skin of its natural oils.
- Exfoliate regularly: Exfoliating removes dead skin cells, preventing them from clogging pores. Choose a gentle exfoliating scrub or chemical exfoliant containing alpha-hydroxy acids (AHAs) or beta-hydroxy acids (BHAs) for optimal results.
- Moisturize wisely: Dry skin can trigger increased oil production. Moisturize regularly with a lightweight, oil-free moisturizer to maintain hydration without clogging pores.
- Hydrate adequately: Drinking plenty of water helps keep the skin hydrated and flushed of toxins, promoting healthy skin function.
- Manage stress: Stress can exacerbate acne. Engage in stress-reducing activities like exercise, yoga, meditation, or spending time in nature.
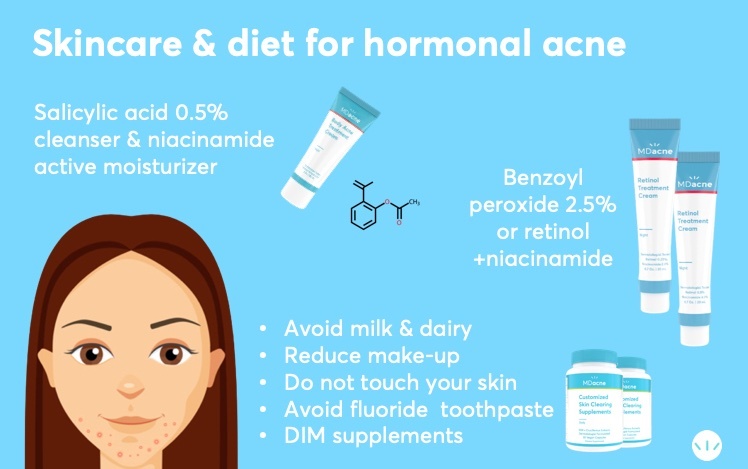
- Diet considerations: While there’s no definitive evidence that diet directly causes acne, some studies suggest that a diet high in processed foods and refined sugars may worsen breakouts. Consuming a balanced diet rich in fruits, vegetables, and whole grains can contribute to overall skin health.
2. Over-the-Counter Treatments: Accessible Solutions
- Benzoyl peroxide: This topical medication effectively kills acne-causing bacteria and reduces inflammation. It’s available in various strengths, ranging from 2.5% to 10%. Start with a lower concentration and gradually increase if tolerated.
- Salicylic acid: This beta-hydroxy acid penetrates pores to dissolve dead skin cells and unclog them. It is available in various forms, including cleansers, toners, and spot treatments.
- Sulfur: This ingredient has antibacterial and anti-inflammatory properties that can help reduce acne and its associated redness. It’s often found in masks, spot treatments, and soaps.
- Tea tree oil: This essential oil has antibacterial and anti-inflammatory effects, making it a natural remedy for acne. Dilute it with a carrier oil like jojoba or almond oil before applying it to the skin.
3. Prescription Treatments: Tailored Solutions for Persistent Acne
For persistent or severe acne, a dermatologist may prescribe stronger medications:
- Topical retinoids: These vitamin A derivatives promote cell turnover, unclog pores, and reduce inflammation. They are available in various strengths and formulations, including gels, creams, and lotions.
- Oral antibiotics: These medications are effective in fighting bacteria and reducing inflammation. However, they are typically used for short periods due to the potential for antibiotic resistance.
- Hormone therapy: In some cases, a dermatologist may recommend low-dose hormone therapy to help balance hormone levels and manage acne.
4. Complementary Therapies: Supporting Skin Health
- Laser therapy: This non-invasive treatment uses a focused beam of light to reduce acne lesions and improve skin texture.
- Chemical peels: These treatments involve applying a chemical solution to the skin to remove dead skin cells and stimulate new cell growth.
- Light therapy: This treatment uses specific wavelengths of light to kill bacteria and reduce inflammation.
FAQs: Addressing Common Concerns
1. Can menopause cause acne even if I never had it before?
Yes, hormonal fluctuations during menopause can trigger acne even in women who have never experienced it previously.
2. How long does menopausal acne last?
The duration of menopausal acne can vary. Some women experience it for a few months, while others may have breakouts for several years.
3. Can I use the same acne treatments I used in my teens?
While some acne treatments used during adolescence may still be effective, others might be too harsh for menopausal skin. It’s best to consult a dermatologist to determine the most appropriate treatment options.
4. Is there a specific diet for menopausal acne?
While there’s no specific diet for menopausal acne, consuming a balanced diet rich in fruits, vegetables, and whole grains can contribute to overall skin health.
5. What are the potential side effects of acne treatments?
Side effects can vary depending on the treatment. Some common side effects include redness, dryness, and irritation. It’s essential to discuss potential side effects with your dermatologist.
Tips for Managing Menopausal Acne:
- Be patient: It may take time to find the right treatment for your specific skin type and concerns.
- Avoid picking or squeezing pimples: This can worsen inflammation and lead to scarring.
- Use sunscreen daily: Sun exposure can exacerbate acne and worsen scarring.
- Consult a dermatologist: A dermatologist can provide personalized advice and treatment recommendations.
Conclusion: Embracing a New Chapter with Clear Skin
Menopausal acne can be a challenging experience, but it’s important to remember that it’s a manageable condition. By understanding the underlying causes, exploring effective treatment options, and adopting healthy lifestyle habits, women can navigate this transition with confidence and clear skin. Consulting a dermatologist is crucial for developing a personalized treatment plan and addressing specific concerns. With the right approach, menopausal acne can be effectively controlled, allowing women to embrace this new chapter in their lives with a radiant glow.



Closure
Thus, we hope this article has provided valuable insights into Navigating the Hormonal Rollercoaster: Acne Treatment During Menopause. We thank you for taking the time to read this article. See you in our next article!